Chesapeake Regional Healthcare has a nationally recognized cardiac program.
Our team of experts treat more than 8,000 patients each year. Whether you need a routine check-up, emergency heart attack treatment or open-heart surgery, we have a specialist to care for you.
To schedule an appointment, please call our Chesapeake office at 757-312-4047 or our Elizabeth City office at 252-335-4890!
Should I see a doctor for my heart concern?
If you experience any of these heart attack symptoms, go to an Emergency Department or call 911 at once:
- Chest pain or discomfort, which may feel like pressure, fullness, aching or squeezing
- Lightheadedness, nausea or vomiting
- Pain or discomfort that spreads to the jaw, neck, arm, shoulder or back
- Shortness of breath
- Weakness or extreme exhaustion
- Women may experience a sharp pain in the neck, arm or back
These lesser-known symptoms may signal that your heart needs a check-up as soon as possible:
- Sweating
- Dizziness or fainting
- Unusual anxiety
- Pain or numbness in one or both arms or legs
- Swelling of the legs, ankles or feet
- Change in skin color
- Ongoing heartburn
Heart disease, which can lead to a heart attack, stroke and heart failure, is the leading cause of death in the United States.
Nearly half of all Americans have at least one of the following three risk factors that play a role in heart disease:
- Smoking
- High blood pressure
- High cholesterol
Obesity, an unhealthy diet, inactivity, tobacco use and consuming too much alcohol are lifestyle risk factors for heart disease. Consider speaking to your provider for a check-up if these apply to you.
Chesapeake Regional offers the best in cardiac care, including:
- A nationally recognized heart program: Because we are an accredited Chest Pain Center, our patients are assured excellent heart care when it is most needed.
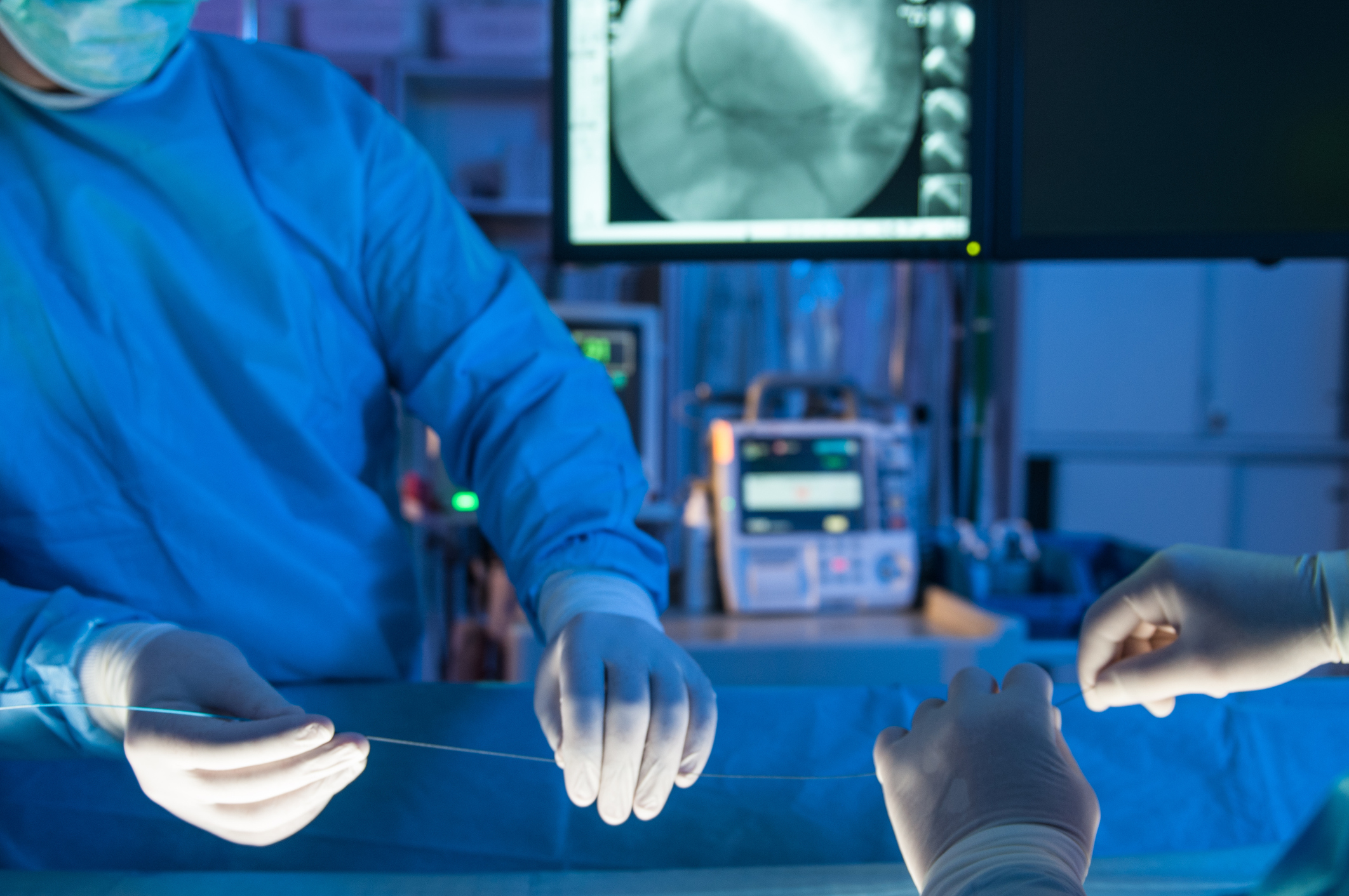
- The quickest treatment: Heart patients at Chesapeake Regional are treated in our state-of-the art cardiac catheterization lab within 90 minutes. That is the highest standard for heart care.
- Coronary Microvascular Dysfunction Studies: Chesapeake Regional Healthcare offers the region's first coronary microvascular dysfunction study, providing accurate diagnosis for patients with chest pain and normal coronary arteries. This innovative testing helps end the cycle of repeated cardiac catheterizations and offers targeted treatment based on proven clinical trial data for better patient outcomes.
- Experience that matters: Our team cares for more than 8,000 heart patients every year. From diagnosis to treatment, our specialists can help with any concern of the heart and blood vessels.
- Advanced ways to diagnose heart disease: We offer the latest diagnostic testing for heart conditions, including Heart Flow. This innovative technology helps our doctors learn more about the heart.
- The latest minimally invasive procedures: We can treat many heart conditions without surgery. We use cardiac catheterization, which requires only a small cut and a shorter recovery time. Chesapeake Regional offers the first fully robotic cardiac catheterization lab in the world.
- Open-heart surgery for those who need it: We offer traditional surgery for more advanced heart disease procedures not done robotically. We offer these surgeries to our patients so that our cardiac offerings are all-inclusive.
Visit Find A Doctor to schedule a consultation with one of our cardiologists, interventional cardiologists, electrophysiologists, or cardiothoracic surgeons.
Services & Specialties
HeartFlow® Analysis
A Personalized Heart Test
Coronary artery disease (CAD) is the leading cause of death for both men and women in the United States. CAD develops when the arteries leading to the heart narrow or become blocked, which may lead to a reduction in blood flow to the heart, causing chest pain, heart attacks and death. Despite being the most common form of heart disease, many of the non-invasive tests available today have low accuracy rates in detecting the disease.
Chesapeake Regional is advancing the diagnosis of CAD with the HeartFlow® Analysis. This non-invasive heart test provides a personalized 3D model of your coronary arteries that shows how each blockage impacts blood flow to your heart. This detailed information, which was previously only available through an invasive procedure, helps your doctor determine the next step in your treatment plan.
Robotic Heart Care
Increased control and accuracy
The Corindus CorPath® GRX System is the first FDA-cleared medical device to bring robotic-assisted precision to minimally invasive coronary and vascular procedures. It essentially functions as an e xtension of the cardiologist's hands, providing a more detailed view and increased stability.
xtension of the cardiologist's hands, providing a more detailed view and increased stability.
What is the CorPath GRX System?
It's the first robotic-assisted system designed to improve precision during angioplasty or PCI procedures. Chesapeake Regional is the first hospital in the region to use the system to perform coronary and vascular procedures.
Robotic Heart Care Announcement
Watch Mark Toland President and CEO of Corindus announce Chesapeake Regional as the world's first fully robotic cardiac catheterization lab. Read about their announcement in our News & Media section.
Chest Pain Center
We're here when you need it most
 Every 33 seconds, someone in the U.S. dies from cardiovascular disease. That's why we established the Chest Pain Center (CPC) within our Emergency Services Department. We ensure that patients receive fast, accurate diagnosis and treatment as soon as they arrive at our doors. The CPC is a collaborative effort involving a multidisciplinary team of board-certified and nationally recognized interventional cardiologists, emergency physicians, a rapid response nurse team, cardiovascular technologists and EMS personnel.
Every 33 seconds, someone in the U.S. dies from cardiovascular disease. That's why we established the Chest Pain Center (CPC) within our Emergency Services Department. We ensure that patients receive fast, accurate diagnosis and treatment as soon as they arrive at our doors. The CPC is a collaborative effort involving a multidisciplinary team of board-certified and nationally recognized interventional cardiologists, emergency physicians, a rapid response nurse team, cardiovascular technologists and EMS personnel.
- We treat an average of 8,000 chest pain-related cases annually.
- We perform an average of 480 urgent and emergent cardiac interventions annually.
- We have a better than average door-to-balloon time (a measurement of the time between when a heart attack patient comes through the door of the emergency room and receives treatment).
- For more than two years we have consistently met a door-to-balloon time of less than 90 minutes - the best in the region.
- Our Cardiac Catheterization Lab is equipped with Philips' digital flat-plane cardiac-vascular X-ray system.
Locations
736 Battlefield Blvd. North
Chesapeake , VA 23320
736 Battlefield Blvd. North
Chesapeake, VA 23320
Awards & Accreditations

2025 NCDR Chest Pain - MI Registry Platinum Performance Achievement